Keeping the Community and Its Economy Healthy 
Since the 1960s, U.S. health centers have provided care in underserved areas regardless of patients' ability to pay. Today, with federal investment from the American Recovery and Reinvestment Act of 2009 (ARRA) and the Affordable Care Act of 2010 (ACA), the number of health centers has reached 1,200.
Much of that federal investment represents bipartisan efforts to address serious access issues-issues highlighted by research such as a 2007 study that estimated 60 million Americans in lower-income rural and urban communities lacked a source of primary care.[1]
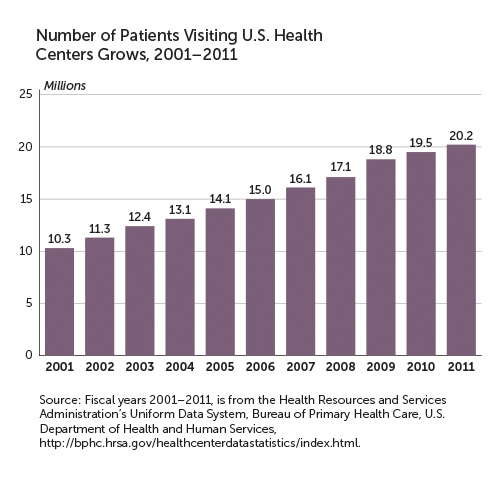
And the investment is paying off. Since 2001, the use of health centers has grown by an impressive 96 percent, and more people are receiving care. (See "Number of Patients Visiting Health Centers Grows, 2001-2011." )
Meeting Needs
Health centers offer care to people who are isolated from traditional medical options because of various factors-for example, where they live, the language they speak, or their complex health-care needs. More than 60 percent of patients are members of racial and ethnic minority groups, and nearly 40 percent have no health insurance. Although one out of every 16 U.S. residents relies on a community health center, the unmet need is still enormous. As a result, health centers plan to double their capacity to serve 40 million patients over the next several years.
Health centers currently provide comprehensive primary and preventive care for over 22 million people annually in more than 9,000 urban and rural communities. Research shows that quality and patient satisfaction are high. One study demonstrated that healthcenter patients received more preventive services than patients of other providers-and better or equal care.[2]
According to a May 2012 White House report, the number of patients receiving care from a community health center increased by nearly 3 million from 2008 to 2011 as a result of Affordable Care Act investments.[3] An additional 1.3 million patients will be served by the end of 2013 thanks to the ACA Capital Development grants awarded in August 2012.
Meanwhile, health centers benefit communities in other ways. In addition to expanding access to care, they stimulate local economies in underserved areas by building or renovating facilities and by adding jobs. Economic benefits result from the capital investment itself, from the center's operations, and from the ability to attract other development projects such as pharmacies, banking facilities, and retail upgrades. In addition, local purchases made by health centers and their employees create ripple effects communitywide.
Economic activity can be calculated in terms of direct, indirect, and induced impact. Direct benefits flow from expanded operations, new facilities, and hiring. Indirect benefits flow from local purchases. Induced benefits occur as local industries grow and household income increases, giving residents more money to spend.
In May 2013, Capital Link, a nonprofit that assists health centers with planning and managing growth, conducted an analysis to assess health centers' national economic impact. It found that the centers collectively generated more than $23.4 billion in total economic activity for their local communities-an increase of 17.5 percent since 2009.[4]
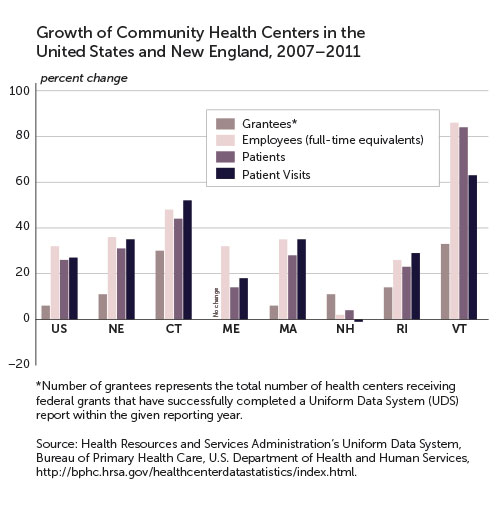
Investment in health centers also creates jobs for which residents may apply. Construction workers are needed first, then new doctors, nurses, administrators, and support personnel. According to the White House report, 131,000 individuals nationwide are employed at health centers, an increase of more than 15 percent since 2009. (See "Growth of Community Health Centers." )
New England Data
Roughly 7 percent of U.S. patients visit community health centers located in New England, and 9 percent of health-center employees work at New England sites.[5] How do the sites benefit their communities economically? Much can be learned from an integrated economic modeling and planning tool called IMPLAN (IMpact analysis for PLANning) that Capital Link uses to assess the multiplier effect of each health center's business operations, job creation, and likely future growth.[6] Consider two New England examples-one in Massachusetts, one in Connecticut.
Codman Square Health Center, in Boston's poorest neighborhood, is Dorchester's largest employer and was contributing more than $31 million annually to the local economy even before a 2011 expansion. As a result of its $18.4 million capital project, Codman Square increased patient access by 56 percent and its staff by 14 percent, generating an additional $27 million in economic impact during the construction period and 178 temporary jobs.[7]
By 2016, or five years following expansion, the health center is expected to have a higher level of economic activity-an estimated total economic impact of $42.9 million per year, with 224 direct, full-time jobs, plus an additional 74 indirect and induced jobs.
Connecticut
Generations Family Health Center offers similar economic benefits to the semirural town of Willimantic, Connecticut, 35 miles from Hartford. The health center has generated more than $14 million annually in total economic impact since 2009 (direct, indirect, and induced) and has employed 100 individuals. The health center completed a new facility in December 2011, doubling capacity to accommodate a 54 percent increase in the number of annual patient visits. As a result of this $10.6 million capital project, Generations created 38 temporary construction jobs and 77 additional permanent jobs. The capital project also provided incremental economic benefits estimated at $15.5 million. By 2016, the economic impact from expanded operations should hit $24.8 million annually.
A Need for Expansion
Many health centers nationwide operate in older buildings-20 years to 110 years old. In a study released by Capital Link in June 2012, 76 percent of health centers indicated they had specific plans to initiate capital projects within the next five years.[8] These projects are estimated to be able to accommodate an additional 6.9 million patients and over 6,600 more providers.
The new and expanded sites go beyond primary health care. They also offer language and culture support in their service areas, with a positive effect on patients' overall well-being. Their community boards help them to identify health needs in their neighborhoods and design effective solutions.
Such solutions may encompass specialty services. Generations Family Health Center, which describes itself as providing "a full continuum of primary health care, oral health care, behavioral health care, and case management and support services for people of all ages," is one example. Conveniently, Generations is located in the same building as ACCESS Agency, which offers behavioral health services. The health center also has a mobile dental program for children and seniors.
Similarly, Codman Square Health Center believes a true "culture of health" is achieved by attending to the whole person and the whole community. To that end, it prioritizes its affiliation with the award-winning Codman Academy, a Boston charter school located within the health center. Codman Square also fosters creative partnerships with organizations that share its mission. One example is Dotwell, a collaboration between the health center and Dorchester House Multi-Service Center offering public-health education, newparent support groups, nutrition classes, computer training, and personal-finance coaching.
Health centers provide services not typically found in other care settings, and they generally operate more efficiently. Federally qualified health centers are paid through a cost-based reimbursement system (the Prospective Payment System, or PPS) that covers a bundle of services for Medicaid and Medicare patients. It lets health centers provide both primary and preventive services, and it ultimately reduces wasteful use of resources. Each year, health centers save more than $1,200 per patient in total health-care costs and achieve $24 billion in annual savings from reduced emergency-room visits, hospital stays, and specialty- care costs.[9]
Because of their success in delivering care, the Health Centers Program is considered one of the most effective federal programs. It continues to receive bipartisan support, most recently through the Consolidated and Further Continuing Appropriations Act of 2013, which provides a $300 million increase in funding compared with 2012. That allows existing health centers to keep up with rising costs in the marketplace and provide for the expansion of care to 1.5 million new patients. At a time when demand is far outpacing capacity, health centers are poised to expand access to care nationwide.
Peg Underhill is Capital Link's marketing and communications manager. She is based in Boston. Contact her at punderhill@caplink.org.
Endnotes
[1] "Primary Care Access: An Essential Building Block of Health Reform" (report, National Association of Community Health Centers, May 2009). [Back to story]
[2] L.E. Goldman et al., "Federally Qualified Health Centers and Private Practice Performance on Ambulatory Care Measures," American Journal of Preventive Medicine 43, no. 2 (2012): 142- 149. [Back to story]
[3] See http://www.whitehouse.gov/sites/default/files/05-01-12_community_health_center_report.pdf. [Back to story]
[4] "The National Economic Impact of Health Centers" (report, Capital Link, Boston, forthcoming). [Back to story]
[5] See http://bphc.hrsa.gov/healthcenterdatastatistics/index.html. [Back to story]
[6] See http://implan.com/V4/Index.php. [Back to story]
[7] The analysis calculates full-time equivalents (FTEs). One FTE is a worker with a 40- hour week; a worker with a 20-hour week is 0.5 FTE. [Back to story]
[8] See Capital Plans and Needs of Health Centers: A National Perspective, http://www.caplink.org/images/stories/Resources/reports/
CapitalNeedsAssessment6.28.12.pdf. [Back to story]
[9] Leighton Ku et al., "Using Primary Care to Bend the Curve: Estimating the Impact of a Health Center Expansion on Health Care Costs" (Geiger Gibson/RCHN Community Health Foundation Research Collaborative Policy Research Brief no. 14, Washington, DC, September 2009), http://sphhs.gwu.edu/departments/healthpolicy/dhp_publications/pub_uploads/
dhpPublication_61D685D5-5056- 9D20-3DDB6CDE10382393.pdf. [Back to story]
Articles may be reprinted if Communities & Banking and the author are credited and the following disclaimer is used: "The views expressed are not necessarily those of the Federal Reserve Bank of Boston or the Federal Reserve System. Information about organizations and upcoming events is strictly informational and not an endorsement."

 About the Authors
About the Authors
Peg Underhill, Capital Link



